Keratoconus – Progressive thinning and distortion of the cornea
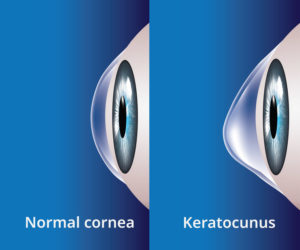 Keratoconus is an eye disease of the cornea: the thin, clear tissue covering the surface of the front of the eye. A normal, healthy cornea is round in shape, but sometimes the cornea can weaken, losing its shape. Instead of a dome, it becomes cone-shaped, preventing clear vision. This is known as keratoconus.
Keratoconus is an eye disease of the cornea: the thin, clear tissue covering the surface of the front of the eye. A normal, healthy cornea is round in shape, but sometimes the cornea can weaken, losing its shape. Instead of a dome, it becomes cone-shaped, preventing clear vision. This is known as keratoconus.
It is a progressive disorder that can either progress rapidly or take years to develop. It may affect only one eye but more commonly occurs in both.
Causes of Keratoconus
The cause of keratoconus is unknown. It is a relatively rare disease – it is estimated that 1 person out of 1,500 is affected – and seems to have genetic components. Keratoconus is most prevalent in those who are near-sighted.
 Many patients who have keratoconus report vigorous eye rubbing. Although it is not proven that eye rubbing can cause or worsen keratoconus, it is probably a good idea to keep from rubbing the front of your eye too much anyway. Many patients with keratoconus also have allergies and eczema, but the link to allergic disease also remains unclear.
Many patients who have keratoconus report vigorous eye rubbing. Although it is not proven that eye rubbing can cause or worsen keratoconus, it is probably a good idea to keep from rubbing the front of your eye too much anyway. Many patients with keratoconus also have allergies and eczema, but the link to allergic disease also remains unclear.
Two theories for keratoconus have been suggested:
- Keratoconus corneas are more easily damaged by minor trauma such as eye rubbing.
- Keratoconus corneas lack the ability to self-repair routine damage easily repaired by normal corneas.
Keratoconus affects people of all races and both sexes. Most patients develop keratoconus in their late teens to early twenties. It can begin at any age, but it is much less common after the age of 30.
There are no preventative measures for keratoconus, but if you develop it, there are many good keratoconus treatment options available.
Keratoconus Treatment
The first symptoms of keratoconus are blurred vision and increased sensitivity to light.
Contact Lenses
In the mildest form of keratoconus, glasses can correct the mild near-sightedness and/or astigmatism caused by keratoconus. Eventually though, keratoconus may progress so far that glasses cannot correct your vision.
As the disorder progresses and the cornea becomes increasingly distorted, specially designed soft lenses often work well.
In more advanced keratoconus, rigid gas permeable (RGP or hard) contact lenses are good choices for vision correction. An RGP contact lens is designed so that its front curve is spherical (to provide undistorted vision) but the back curves are tailored so the lens stays on the irregular cornea.
Fitting contact lenses on a keratoconus cornea is delicate and time-consuming. A poorly fitting lens can cause scarring on the eye surface as well as discomfort and poor vision. Correct fitting will require frequent follow-up visits to fine-tune. In some cases, many months. Lenses also need to be refitted regularly to maintain good vision and lens comfort.
Advanced Keratoconus Treatment
In advanced cases, the cornea wears down at the very point of the cone shape. If this happens, you may need to consider other keratoconus treatment and there are good options available.
Corneal Collagen Cross-linking
Corneal collagen cross-linking works by saturating the cornea with custom-made riboflavin drops which are then activated by ultraviolet light over a 30-minute session. This treatment increases the collagen cross-links which are the natural’ “anchors” within the cornea. These anchors are responsible for preventing the cornea from bulging out and becoming steep and irregular and collagen cross-linking will strengthen them.
We don’t perform corneal collagen cross-linking at John O’Connor Optometrists, but should we think this is a good keratoconus treatment option for you, we can refer you to see an ophthalmologist, either privately or through the public hospital system.
Collagen cross-linking is not a cure for keratoconus. It does not reverse any change that has already occurred, but it can arrest progression and further deterioration in vision. Glasses or contact lenses will still be needed following a cross-linking treatment, but with a change in prescription.
Corneal Transplants
Should keratoconus progress so much that contact lens wear becomes unsuccessful or the cornea becomes scarred, then a corneal transplant may be indicated.
Although there is some risk of tissue rejection, it is relatively low. Few people may welcome the need for this procedure, but corneal transplants do enjoy a high rate of success.
The main limitation is the number of donated corneas – the NZ National Eye Bank relies on organ donors to provide the sight-restoring corneal tissue. Most often, patients will still need to wear contact lenses after the surgery.
Keratoconus Diagnosis
Always see your eye care professionals at John O’Connor Optometrists immediately if you have any sudden changes in vision. This includes darkening around the edges of your vision, dark spots in front of your eyes, halos around bright lights, a loss of vision in one part of your field of sight or any other noticeable change. If your child or teenager has vision problems that cannot be corrected to 20/20 with glasses, they should be evaluated by an eye care professional with experience in diagnosing and treating keratoconus.
Regular eye examinations are a must. Keratoconus can be diagnosed in a slit-lamp examination or by corneal topography. It is during these exams that your health care provider has a chance to detect any conditions like keratoconus before they become a bigger problem. Once-a-year check-ups are instrumental in maintaining health vision over your lifetime. Full eye exams start from $65 and you can get an eye test at either our Newmarket or Henderson optometry practice. Call 09 522 1283 or 09 836 1731 to book an appointment with one of our Auckland optometrists.

